DYSLIPIDEMIA
Coronary Heart Disease abbreviated as “CHD” is a pathologic condition in which a fatty wax resembling substance called plaque builds up and accumulate on the inner walls of the arteries supplementing the heart with oxygen-rich blood. These heart arteries are called the coronary arteries.
Plaques narrow these arteries and reduce blood flow to your heart muscle. Reduced blood flow can cause chest pain, especially when you’re doing any activity like sports or climbing stairs. This can sometimes even happen at rest. Eventually, an area of plaque can rupture (break open). This causes a blood clot to form on the surface of the plaque. This condition is called “Atherosclerosis”
If the clot becomes large enough, it can block the flow of oxygen-rich blood to the portion of the heart that the artery feeds. Blocked blood flow to the heart muscle causes a heart attack or even a myocardial infarction known as heart muscle death.
Coronary heart disease risk factors: There are many known CHD risk factors. Some risk factors can be controlled by the patient and others not.
Risk factors you can control and modify include:
- High blood cholesterol and triglyceride levels
- High blood pressure
- Diabetes and prediabetes. Prediabetes is also known as insulin resistance
- Smoking
- Overweight and obesity – Unhealthy diet
- Lack of physical activity
- Stress
The risk factors that patients can’t control are:
- Age
- Gender
- Family history of CHD
The risk of CHD and heart attack increases with the number of risk factors patients have as well as their severity.
Some risk factors have a greater risk of CHD and heart attack than others, these include mainly smoking diabetes and hypertension.
Cholesterol as a CHD risk factor
High blood cholesterol is a condition in which the patient blood has too much cholesterol. The higher the cholesterol level, the greater the risk of coronary heart disease (CHD) and heart attack.
We are not going to go through the normal values in this topic, but kindly revert to your healthcare provider if your cholesterol levels are higher than normal when you get your results from the laboratory.
Cholesterol travels through the bloodstream in small packages called lipoproteins. Two major kinds of lipoproteins carry cholesterol throughout your body:
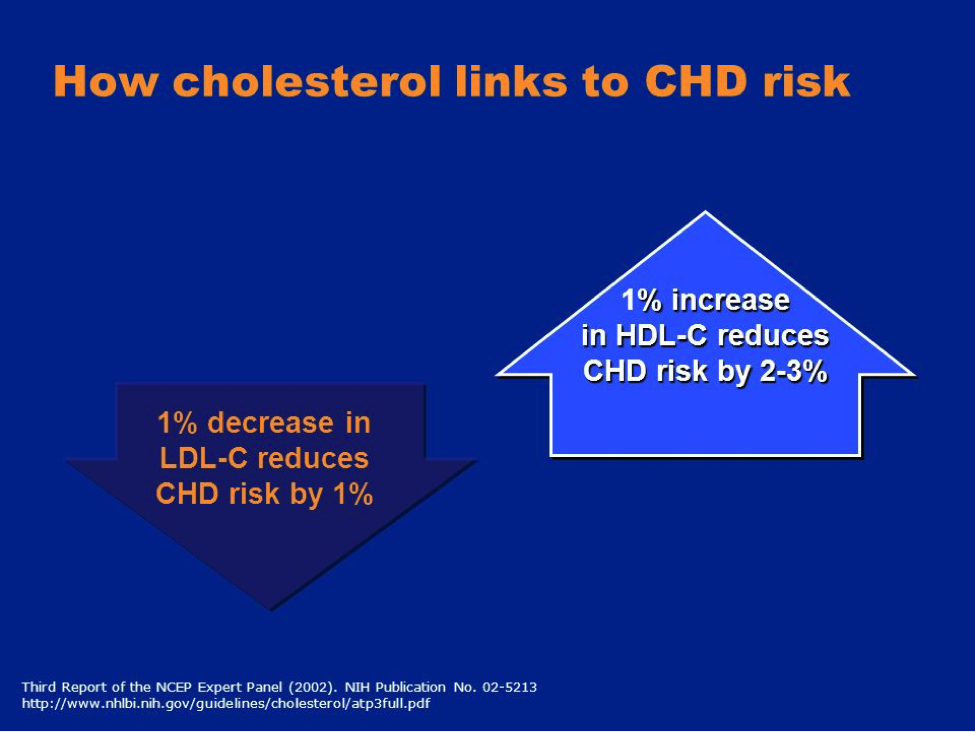
- Low-density lipoproteins (LDL). LDL cholesterol sometimes is called “bad” cholesterol. This is because it carries cholesterol to tissues, including the heart arteries where they get stuck there and contribute to the process of atherosclerosis described above. A high LDL cholesterol level raises the risk of CHD.
- High-density lipoproteins (HDL). HDL cholesterol sometimes is called “good” cholesterol. This is because it helps remove cholesterol from the arteries through a process called reverse cholesterol transport. A low HDL cholesterol level raises the risk of CHD
- Healthy levels of both LDL and HDL cholesterol will prevent plaque from building up in the arteries. Routine blood tests can show whether blood cholesterol levels are healthy or not.
- Oxidation and bad cholesterol LDL
- In patients with hypercholesterolemia, excess LDL infiltrates the artery
- The higher the LDL level in the bloodstream, the more LDL works its way into the artery walls. As the LDL cholesterol accumulates, it becomes oxidized (that is, it combines with free radical oxygen coming from excess oxidative stress), provoking an inflammatory reaction that results in the formation of plaques, which are made of cholesterol-rich fatty deposits, proteins and other substances of inflammation. Other factors, such as smoking and high blood pressure, can further damage and injure the artery wall and aggravate inflammation.
Hence one important way in managing high LDL levels is to decrease the levels of the oxidized LDL particles and not just the high levels of LDL.
Decreasing levels of oxidized LDL particles is core to the treatment of atherosclerosis
Management of high levels of cholesterol / LDL – Lifestyle modification
The high cholesterol patient treatment plan
Work with your healthcare provider on an agreed upon plan that works best for you and your family. For support, encourage your whole family to join you in your heart-healthy lifestyle.
This includes:
- Making sure you understand what cholesterol is and how to manage it.
- Knowing your risks for heart disease and how to reduce your risk especially by working on modifiable risk factors.
- Stop smoking.
- Eating a heart-healthy diet by staying away from food rich in fats, trans fats, fried food, fast food and consuming more vegetables and fruits
- Getting enough physical activity.
- Reaching and maintaining a healthy weight.
Since high blood pressure and diabetes are also important risk factors for CHD, talk to your healthcare provider about your blood pressure and blood sugar to make sure they are in check and managed properly too.
Lipid Lowering Medicines: STATINS
LDL-C remains the primary target of therapy in most strategies of dyslipidemia management
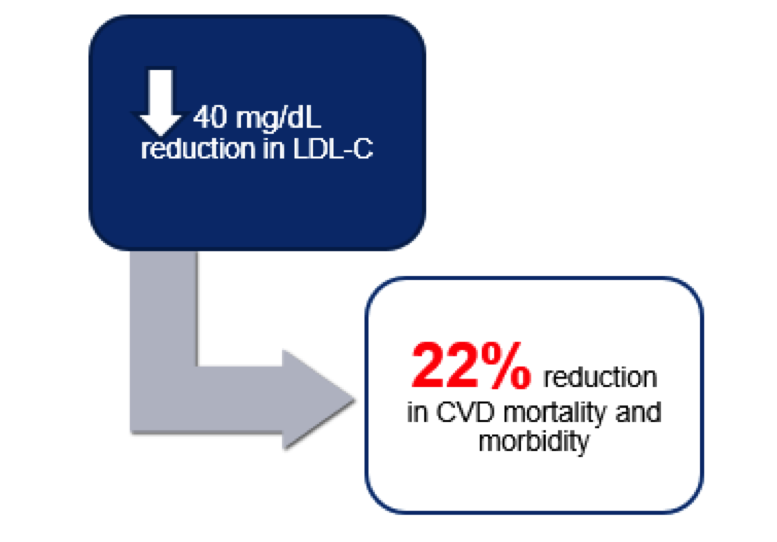
Improved Cardiovascular Outcome is seen with a drop in LDL-C levels. As an established example, a reduction of 40 mg/dL in LDL-C leads to 22% reduction in Cardio Vascular Disease mortality and morbidity (figure 1). Improving your good cholesterol levels HDL-C may also have the same good heart disease reduction effect (Figure 2)
The majority of medical guidelines advise patients to modify their lifestyle before starting them on medicines called statins. A naturally occurring statin called Red Yeast Rice acts like statins and will lower your bad cholesterol levels when supplemented regularly.
Also and on another hand and in patients taking statins or red yeast rice, it has been shown that Co-enzyme Q10 (CoQ10) which is involved in energy production of the cell is decreased. CoQ10 reduces myopathy (muscle weakness and damage) associated with statin use. On another hand, CoQ10 has antioxidant properties regenerating active forms of vitamin C and E. when CoQ10 binds to the bad cholesterol LDL, it makes it more resistant to oxidation, therefore less capable of digging under the artery fragile layer of cells called endothelium, and hence protects the artery from producing foam cells which are the first step in the development of the atherosclerotic plaque.
